Psychotic Break: Symptoms, Triggers And Treatments

Understanding Psychotic Breaks
Psychotic breaks can be distressing and disruptive experiences for individuals who go through them. Understanding what a psychotic break is and recognizing its symptoms are crucial for early intervention and effective treatment.
What is a Psychotic Break?
A psychotic break, also known as a psychotic episode or psychotic episode, refers to a period of time when an individual experiences a loss of touch with reality. During a psychotic break, a person may have difficulty distinguishing between what is real and what is not. This can lead to unusual thoughts, perceptions, and behaviors that are significantly different from their usual functioning.
Psychotic breaks can occur as a result of various mental health conditions, such as schizophrenia, bipolar disorder, or severe depression. They can also be triggered by external factors, such as extreme stress or trauma. It's important to note that a psychotic break is not a diagnosis in itself but rather a symptom of an underlying mental health condition.
Symptoms of a Psychotic Break
The symptoms of a psychotic break can vary from person to person and may differ based on the underlying cause. Some common symptoms include:
- Hallucinations: Seeing, hearing, or feeling things that are not actually present.
- Delusions: Holding false beliefs that are not based on reality.
- Disorganized thinking: Difficulty organizing thoughts and expressing oneself coherently.
- Disrupted speech: Speaking in a way that is illogical, incoherent, or incomprehensible.
- Paranoia: Feeling excessively suspicious or fearful of others.
- Social withdrawal: Avoiding social interactions and isolating oneself from others.
- Emotional instability: Experiencing intense and unpredictable emotional states.
It's important to note that these symptoms can be distressing and may significantly impact an individual's daily functioning and overall well-being. If you or someone you know is experiencing these symptoms, it is crucial to seek professional help for an accurate diagnosis and appropriate treatment.
Understanding the nature of psychotic breaks and recognizing the associated symptoms are crucial steps in providing the necessary support and interventions for individuals experiencing these episodes. Early identification and treatment can greatly improve outcomes and help individuals regain stability and manage their mental health effectively.
Common Triggers of Psychotic Breaks
Psychotic breaks can be triggered by various factors, and understanding these triggers is essential for managing and preventing episodes. Here are three common triggers that can contribute to psychotic breaks: stress and trauma, substance abuse, and sleep deprivation.
Stress and Trauma
Stress and trauma are significant triggers for psychotic breaks. Experiencing high levels of stress or going through traumatic events can disrupt the delicate balance of the mind, leading to a breakdown in reality. These triggers can be both acute, such as a sudden traumatic event, or chronic, such as ongoing stressors in daily life.
It is crucial to recognize and manage stress and trauma to reduce the risk of psychotic breaks. Techniques such as stress management, therapy, and engaging in stress-reducing activities like mindfulness or exercise can help individuals cope with stress and trauma more effectively.
Substance Abuse
Substance abuse, including the use of drugs and alcohol, can greatly increase the risk of psychotic breaks. Certain substances, such as hallucinogens or stimulants, can directly induce hallucinations, delusions, and other symptoms associated with psychotic breaks. Prolonged substance abuse can also contribute to changes in brain chemistry, making individuals more susceptible to psychotic episodes.
Here is a table displaying the risk associated with substance abuse:
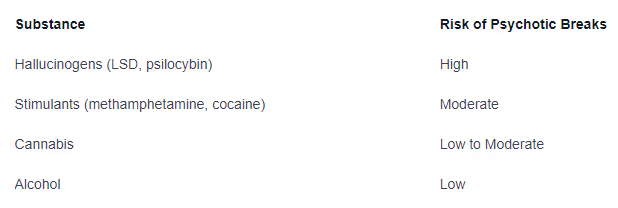
Avoiding substance abuse and seeking help for addiction or substance use disorders is vital for managing and preventing psychotic breaks.
Sleep Deprivation
Lack of adequate sleep can have a profound impact on mental health and increase the risk of psychotic breaks. Sleep deprivation disrupts brain functions, impairs cognitive abilities, and weakens the ability to cope with stress. Over time, chronic sleep deprivation can trigger or worsen existing mental health conditions, including psychotic disorders.
Here is a table showing the recommended sleep duration for different age groups:

Establishing a healthy sleep routine, practicing good sleep hygiene, and addressing any underlying sleep disorders can help regulate sleep patterns and reduce the risk of psychotic breaks.
By understanding and managing these common triggers - stress and trauma, substance abuse, and sleep deprivation - individuals can take proactive steps in preventing and minimizing the occurrence of psychotic breaks. It is crucial to seek professional help and support to develop personalized strategies for managing these triggers and maintaining mental well-being.
Managing Psychotic Break Symptoms
When it comes to managing psychotic break symptoms, a comprehensive treatment plan is essential. This typically involves a combination of medication, psychiatric treatment, psychotherapy and counseling, as well as lifestyle changes and self-care practices. Let's explore each of these approaches in more detail.
Medication and Psychiatric Treatment
Medication plays a vital role in managing psychotic break symptoms. Antipsychotic medications are commonly prescribed to help alleviate symptoms such as hallucinations, delusions, and disorganized thinking. These medications work by balancing the chemicals in the brain that are associated with psychosis.
It's important to note that medication should always be prescribed and monitored by a qualified psychiatrist or healthcare professional. The type and dosage of medication can vary depending on the individual and their specific symptoms. Regular follow-up appointments are crucial to assess the effectiveness of the medication and make any necessary adjustments.
Psychotherapy and Counseling
Psychotherapy and counseling are valuable components of treatment for individuals experiencing psychotic break symptoms. These therapies provide a supportive and safe environment to explore and address the underlying causes and triggers of the psychotic break.
Cognitive Behavioral Therapy (CBT) is often recommended for individuals with psychosis. CBT helps individuals identify and challenge distorted thoughts and beliefs, develop coping strategies, and improve problem-solving skills. Other therapeutic approaches, such as family therapy or group therapy, may also be beneficial in providing additional support and understanding.
Lifestyle Changes and Self-Care
In addition to medication and therapy, lifestyle changes and self-care practices can significantly contribute to managing psychotic break symptoms. Adopting a healthy lifestyle that includes regular exercise, adequate sleep, and a balanced diet can have a positive impact on overall well-being.
Engaging in stress-reduction techniques, such as mindfulness meditation, deep breathing exercises, and relaxation techniques, can help individuals manage stress and reduce the risk of triggering symptoms. It's important to find activities that promote relaxation and provide a sense of calm.
Maintaining a structured daily routine and engaging in meaningful activities can also be helpful. Setting realistic goals, practicing good time management, and avoiding excessive stress can contribute to overall stability and reduce the likelihood of experiencing a psychotic break.
Self-care practices, such as engaging in hobbies, practicing good hygiene, and surrounding oneself with a supportive network of friends and family, are essential for maintaining emotional well-being. Seeking support from others who have experienced similar challenges, such as through support groups or online communities, can also provide valuable insights and encouragement.
By incorporating a multi-faceted approach that includes medication, psychiatric treatment, psychotherapy and counseling, as well as lifestyle changes and self-care practices, individuals can effectively manage psychotic break symptoms and work towards long-term recovery. It's important to consult with healthcare professionals to develop a personalized treatment plan that addresses individual needs and goals.
Identifying Personal Triggers
When it comes to managing and preventing psychotic breaks, it's important to identify and understand your personal triggers. By recognizing the factors that contribute to these episodes, you can take proactive steps to minimize their impact. In this section, we will explore three strategies for identifying personal triggers: self-reflection and awareness, keeping a trigger journal, and seeking professional guidance.
Self-Reflection and Awareness
Self-reflection and self-awareness play a vital role in identifying personal triggers for psychotic breaks. Taking the time to reflect on your thoughts, emotions, and experiences can provide valuable insights into patterns and triggers. Ask yourself questions such as:
- What situations or events tend to provoke intense emotional responses?
- Are there certain people, places, or activities that consistently lead to heightened stress levels?
- Do specific thoughts or beliefs trigger feelings of anxiety or distress?
By examining your experiences and emotions, you can start to identify potential triggers and gain a better understanding of how they impact your mental well-being.
Keeping a Trigger Journal
Keeping a trigger journal can be an effective tool for tracking and identifying personal triggers. In your journal, record any significant experiences, emotions, or events that occur before or during a psychotic break. Be sure to include details such as:
- Date and time of the event
- Description of the situation or event
- Thoughts, emotions, and physical sensations experienced
- Any specific triggers that you believe contributed to the episode
Maintaining a trigger journal allows you to identify recurring patterns and trends over time. This information can be valuable when discussing your experiences with healthcare professionals and developing personalized treatment plans.
Seeking Professional Guidance
While self-reflection and journaling are valuable strategies, seeking professional guidance is essential for a comprehensive understanding of your personal triggers. Mental health professionals, such as psychiatrists or psychologists, are trained to help individuals identify and manage triggers associated with psychotic breaks.
Through therapy sessions, mental health professionals can guide you in exploring your experiences, emotions, and thought patterns. They can provide you with the tools and techniques to recognize and cope with triggers effectively. Additionally, they can offer personalized strategies and interventions tailored to your specific needs.
Remember, seeking professional guidance is not a sign of weakness but rather a proactive step towards better mental health. Mental health professionals can provide the necessary support and guidance to help you identify and manage your personal triggers effectively.
By engaging in self-reflection, maintaining a trigger journal, and seeking professional guidance, you can gain valuable insights into your personal triggers for psychotic breaks. This knowledge empowers you to take proactive steps in managing your mental health and minimizing the impact of triggers on your well-being.
Holistic Approaches to Treatment
In addition to traditional medical and therapeutic interventions, there are holistic approaches that can be beneficial in managing psychotic break symptoms and promoting overall well-being. These approaches focus on the interconnection between the mind, body, and social support systems. Here are three holistic approaches that can complement traditional treatments:
Exercise and Physical Health
Regular exercise and taking care of one's physical health can have a positive impact on mental well-being. Engaging in physical activity releases endorphins, which are natural mood boosters. Exercise can also help reduce stress and anxiety, improve sleep, and enhance overall cognitive function.
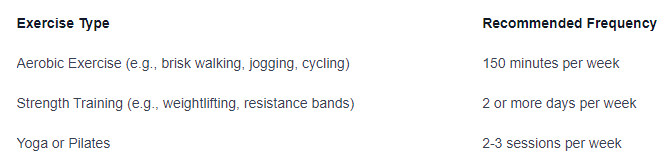
It's important to consult with a healthcare professional before starting any new exercise regimen, especially if you have any underlying health conditions.
Mindfulness and Meditation
Practicing mindfulness and meditation can help individuals with psychotic break symptoms manage their thoughts and emotions. Mindfulness involves being fully present and aware of the present moment, without judgment. Meditation techniques, such as deep breathing exercises and guided imagery, can promote relaxation and reduce stress.
Mindfulness and Meditation Techniques
Mindful breathing exercises
Body scan meditation
Guided visualization
Loving-kindness meditation
Incorporating mindfulness and meditation into daily routines, even for just a few minutes, can provide a sense of calm and improve mental clarity.
Support Networks and Peer Groups
Building a strong support network and connecting with others who have experienced similar challenges can be invaluable in managing psychotic break symptoms. Support networks can include family, friends, support groups, and peer groups. Sharing experiences, offering and receiving support, and learning from others can foster a sense of belonging and reduce feelings of isolation.
Support Network and Peer Group Options
Family and close friends
Support groups for individuals with mental health conditions
Peer support programs
Online communities and forums
Engaging in supportive relationships and participating in group activities can provide emotional validation, practical advice, and a sense of community.
By incorporating these holistic approaches into one's treatment plan, individuals with psychotic break symptoms can enhance their overall well-being and complement traditional treatments. It's important to remember that these approaches should be used in conjunction with professional guidance and support.
Conclusion
Psychotic breaks can have a significant impact on an individual's mental health and overall well-being. By understanding the common triggers and identifying personal triggers, individuals can take proactive steps to manage and prevent psychotic breaks. Treatment for psychotic break symptoms typically involves a combination of medication, psychiatric treatment, psychotherapy and counseling, as well as lifestyle changes and self-care practices. Additionally, incorporating holistic approaches such as exercise, mindfulness, and support networks can complement traditional treatments and enhance overall well-being.
It's important to remember that seeking professional help is crucial in managing psychotic break symptoms effectively. With the right treatment plan and support system in place, individuals with psychotic break symptoms can work towards long-term recovery and improved mental health. By taking a comprehensive approach that addresses physical, psychological, social, and spiritual aspects of well-being, individuals can achieve a more balanced and fulfilling life. Remember that you are not alone in your journey towards better mental health - reach out for help when you need it.
