Types of Eating Disorders

Understanding Eating Disorders
Eating disorders are complex mental health conditions that affect a person's relationship with food and their body. They often involve disturbances in eating behaviors, thoughts, and emotions. Understanding the basics of eating disorders can shed light on their impact and the need for support and treatment.
What are Eating Disorders?
Eating disorders encompass a range of conditions characterized by abnormal eating habits and attitudes towards food and body weight. They can affect individuals of any gender, age, or background. The most commonly known types of eating disorders include anorexia nervosa, bulimia nervosa, and binge eating disorder. However, there are other specified feeding or eating disorders (OSFED) that may not meet the specific diagnostic criteria for these three but still involve significant disordered eating patterns.
Eating disorders are not simply about food or weight; they are complex mental health issues influenced by a combination of biological, psychological, and sociocultural factors. They often manifest as a coping mechanism for underlying emotional distress, low self-esteem, perfectionism, or feelings of lack of control.
Prevalence and Impact of Eating Disorders
Eating disorders are more common than many people realize. They affect millions of individuals worldwide and can have severe physical, emotional, and social consequences. Here are some key facts about the prevalence and impact of eating disorders:
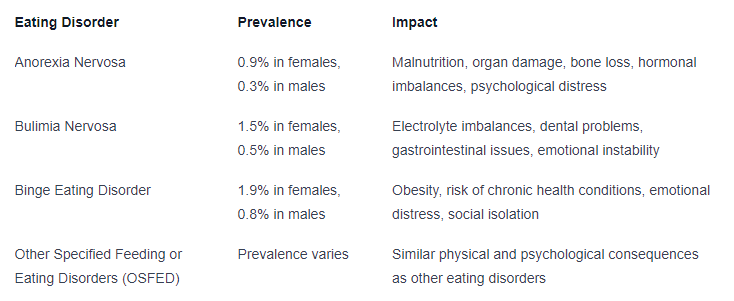
It is important to remember that these statistics only provide a general understanding of prevalence and impact. Eating disorders can affect individuals differently, and each person's experience is unique.
By increasing awareness and understanding of eating disorders, we can promote early identification, intervention, and support. Recognizing the signs and symptoms of eating disorders is crucial in order to seek appropriate professional help and provide compassionate support to individuals who are battling these challenging conditions.
Anorexia Nervosa
Anorexia nervosa is a serious eating disorder characterized by extreme and persistent restriction of food intake, resulting in significantly low body weight. It is accompanied by an intense fear of gaining weight and a distorted body image. Understanding the symptoms, diagnostic criteria, causes, and treatment options for anorexia nervosa is crucial in addressing and supporting individuals affected by this disorder.
Symptoms and Diagnostic Criteria
Anorexia nervosa involves a range of physical, emotional, and behavioral symptoms. The diagnostic criteria for anorexia nervosa, as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), include:
- Restriction of energy intake leading to significantly low body weight.
- An intense fear of gaining weight or persistent behavior that interferes with weight gain.
- Disturbance in the way one's body weight or shape is experienced, resulting in undue influence on self-evaluation.
Common symptoms of anorexia nervosa may include:
Symptom
Excessive weight loss
Preoccupation with food, calories, and dieting
Avoidance of eating meals or certain types of food
Intense fear of becoming fat
Distorted body image
Excessive exercise
Social withdrawal
Irregular or absent menstrual cycles (in females)
Causes and Risk Factors
The causes of anorexia nervosa are complex and multifactorial. They can include a combination of genetic, biological, psychological, and environmental factors. Some known risk factors for developing anorexia nervosa include:
Risk Factor
Genetic predisposition
Perfectionism and high self-expectations
Body dissatisfaction
History of dieting or weight-related teasing
Psychological factors such as low self-esteem and impulsivity
Cultural and societal pressures emphasizing thinness
Treatment Options
Treating anorexia nervosa requires a multidisciplinary approach involving medical, nutritional, and psychological interventions. The primary goals of treatment are to restore weight, address any underlying psychological issues, and promote healthy eating habits. Treatment options for anorexia nervosa may include:
- Medical Monitoring: Regular medical check-ups to assess and manage any medical complications associated with anorexia nervosa, such as electrolyte imbalances, cardiac issues, and malnutrition.
- Nutritional Rehabilitation: Working with a registered dietitian to develop a structured meal plan that promotes weight restoration and meets the nutritional needs of the individual.
- Psychotherapy: Individual, family, or group therapy to address the underlying psychological factors contributing to anorexia nervosa. Cognitive-behavioral therapy (CBT) is often used to challenge distorted thoughts and behaviors related to food and body image.
- Medication: In some cases, medication may be prescribed to address co-occurring mental health conditions, such as depression or anxiety.
- Supportive Care: Creating a supportive environment that involves family, friends, and professionals to provide ongoing support and encouragement throughout the recovery process.
It is important to note that treatment approaches may vary based on individual needs and the severity of the condition. Early intervention and a comprehensive treatment plan can significantly improve the chances of recovery for individuals with anorexia nervosa.
Bulimia Nervosa
Bulimia Nervosa is a serious eating disorder characterized by a cycle of binge eating followed by compensatory behaviors, such as self-induced vomiting, excessive exercise, or the misuse of laxatives. This section will explore the symptoms and diagnostic criteria, causes and risk factors, as well as treatment options for Bulimia Nervosa.
Symptoms and Diagnostic Criteria
Individuals with Bulimia Nervosa often experience recurrent episodes of binge eating, which involve consuming a large amount of food in a short period, accompanied by a perceived loss of control. This behavior is followed by attempts to prevent weight gain through purging or other compensatory behaviors.
The diagnostic criteria for Bulimia Nervosa include:
- Recurrent episodes of binge eating, characterized by:
- Eating an unusually large amount of food within a discrete period.
- Feeling a lack of control over eating during the episode.
- Recurrent inappropriate compensatory behaviors to prevent weight gain, such as:
- Self-induced vomiting.
- Excessive exercise.
- Misuse of laxatives, diuretics, or other medications.
- The presence of binge eating and compensatory behaviors at least once a week for three months.
- Self-evaluation that is unduly influenced by body shape and weight.
- The disturbance does not occur exclusively during episodes of Anorexia Nervosa.
Causes and Risk Factors
The causes of Bulimia Nervosa are complex and can involve a combination of genetic, environmental, and psychological factors. Some common risk factors include:
- Genetics: Having a family history of eating disorders or other mental health conditions may increase the risk of developing Bulimia Nervosa.
- Psychological Factors: Low self-esteem, perfectionism, body dissatisfaction, and a history of trauma or abuse can contribute to the development of Bulimia Nervosa.
- Cultural and Social Pressures: Societal emphasis on thinness, media influences, and societal expectations regarding body image can contribute to the development of disordered eating behaviors.
Treatment Options
Treating Bulimia Nervosa typically involves a multidimensional approach that addresses the physical, psychological, and nutritional aspects of the disorder. Some common treatment options include:
- Psychotherapy: Cognitive Behavioral Therapy (CBT) is often used to help individuals with Bulimia Nervosa challenge negative thoughts and develop healthier coping mechanisms. Interpersonal Psychotherapy (IPT) and Dialectical Behavior Therapy (DBT) may also be effective.
- Nutritional Counseling: Working with a registered dietitian who specializes in eating disorders can help individuals develop a balanced approach to food and establish regular eating patterns.
- Medication: In some cases, medications such as antidepressants may be prescribed to address co-occurring mental health conditions that often accompany Bulimia Nervosa.
- Support Groups: Joining support groups or participating in group therapy can provide individuals with a sense of community and support during their recovery journey.
It's important to note that early intervention and seeking professional help are crucial for effective treatment and recovery from Bulimia Nervosa. With the right support and treatment, individuals can overcome this eating disorder and improve their overall well-being.
Binge Eating Disorder
Binge Eating Disorder (BED) is a serious eating disorder characterized by recurrent episodes of consuming large quantities of food within a short period, accompanied by a feeling of loss of control. Individuals with BED often experience distress and guilt following these episodes, which can significantly impact their overall well-being and quality of life.
Symptoms and Diagnostic Criteria
To be diagnosed with Binge Eating Disorder, an individual must meet the following criteria:
- Recurrent episodes of binge eating, characterized by:
- Eating a larger amount of food than most people would eat in a similar timeframe.
- Feeling a lack of control over their eating during the episode.
- Binge eating episodes are associated with at least three of the following:
- Eating more rapidly than usual.
- Eating until feeling uncomfortably full.
- Eating large amounts of food when not physically hungry.
- Eating alone due to embarrassment or shame.
- Feeling disgusted, depressed, or guilty after the binge.
- Binge eating occurs, on average, at least once a week for three months.
- The binge eating is not associated with the regular use of inappropriate compensatory behaviors, such as purging or excessive exercise, as seen in bulimia nervosa.
Causes and Risk Factors
The exact causes of Binge Eating Disorder are not fully understood. However, several factors may contribute to its development, including:
- Genetics: There may be a genetic predisposition to developing eating disorders, including Binge Eating Disorder.
- Psychological Factors: Individuals with BED often have difficulties with emotional regulation, body image, or low self-esteem. Stress, trauma, or other psychological issues may also play a role.
- Sociocultural Factors: Cultural pressures that emphasize thinness or place a strong emphasis on appearance can contribute to the development of Binge Eating Disorder.
- Dieting and Restrictive Eating: Restrictive eating patterns or cycles of dieting followed by overeating can increase the risk of developing BED.
Treatment Options
Treating Binge Eating Disorder typically involves a comprehensive approach that may include a combination of the following:
- Psychotherapy: Cognitive-Behavioral Therapy (CBT) has been found to be effective in addressing the underlying psychological factors and helping individuals develop healthier coping strategies.
- Medications: Certain medications, such as selective serotonin reuptake inhibitors (SSRIs), may be prescribed to help reduce binge eating episodes and manage any associated mood disorders.
- Nutritional Counseling: Working with a registered dietitian can help individuals establish regular eating patterns, develop a healthy relationship with food, and address any nutritional imbalances.
- Support Groups: Joining support groups or participating in group therapy sessions can provide individuals with BED a sense of community and understanding, as well as additional tools for managing their disorder.
It's important to seek professional help if you or someone you know is struggling with Binge Eating Disorder. With appropriate treatment and support, individuals with BED can work towards recovery and improve their overall well-being.
Other Specified Feeding or Eating Disorders (OSFED)
In addition to anorexia nervosa, bulimia nervosa, and binge eating disorder, there are other specified feeding or eating disorders (OSFED) that fall under the broader category of eating disorders. OSFED encompasses a range of disordered eating behaviors and patterns that do not meet the specific diagnostic criteria for the aforementioned disorders.
Symptoms and Diagnostic Criteria
OSFED is a diagnosis given to individuals who exhibit symptoms of disordered eating but do not meet the full criteria for anorexia nervosa, bulimia nervosa, or binge eating disorder. The specific symptoms and diagnostic criteria for OSFED can vary, but some common examples include:
- Atypical anorexia nervosa: Individuals who restrict their food intake and exhibit a significant weight loss, but their weight remains within or above the normal range.
- Bulimia nervosa of low frequency and/or limited duration: Individuals who engage in episodes of binge eating and compensatory behaviors less frequently than required for a diagnosis of bulimia nervosa.
- Night eating syndrome: Individuals who consume a significant portion of their daily caloric intake during nighttime hours, often waking up to eat or having difficulty falling asleep without eating.
- Purging disorder: Individuals who regularly engage in purging behaviors, such as self-induced vomiting or misuse of laxatives, diuretics, or other medications, without binge eating episodes.
- Other specified feeding or eating disorder of clinical severity: Individuals who display significant distress or impairment related to their eating behaviors but do not meet the criteria for any specific eating disorder.
Causes and Risk Factors
The causes and risk factors for OSFED are similar to those of other eating disorders. They can include a combination of genetic, biological, psychological, and environmental factors. These may include:
- Genetic predisposition and family history of eating disorders or mental health conditions.
- Biological factors such as imbalances in brain chemicals and hormones.
- Psychological factors like low self-esteem, body dissatisfaction, and perfectionism.
- Cultural influences that emphasize thinness or promote unrealistic body ideals.
- Traumatic experiences, such as childhood abuse or bullying.
It's important to note that OSFED can affect individuals of any gender, age, or background.
Treatment Options
Treatment for OSFED typically involves a multidisciplinary approach that addresses the physical, psychological, and nutritional aspects of the disorder. The specific treatment options may vary depending on the individual's symptoms, needs, and preferences. Some common approaches include:
- Psychotherapy: Various forms of therapy, such as cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), or interpersonal therapy (IPT), can help individuals address the underlying issues contributing to their disordered eating behaviors.
- Nutritional counseling: Working with a registered dietitian can help individuals establish a balanced and healthy approach to eating, while addressing any specific nutritional deficiencies or concerns.
- Medical monitoring: In some cases, medical professionals may monitor the individual's physical health and provide necessary interventions to address complications associated with disordered eating.
- Support groups or group therapy: Participating in support groups or group therapy sessions can provide individuals with a sense of community, understanding, and encouragement from others who have similar experiences.
The treatment approach for OSFED should be tailored to the individual's unique needs and may involve a combination of these interventions.
By recognizing the existence of OSFED and understanding its symptoms, causes, and treatment options, individuals and healthcare professionals can better address and support those who may not fit neatly into the diagnostic criteria of other specific eating disorders.
Seeking Help and Support
When it comes to eating disorders, seeking help and support is crucial for recovery. Identifying warning signs, understanding the role of mental health professionals, and accessing appropriate resources are important steps in the journey towards healing.
Identifying Warning Signs
Recognizing the warning signs of an eating disorder is the first step in seeking help. While the specific symptoms may vary depending on the type of eating disorder, there are common signs to be aware of:
Common Warning Signs
Drastic weight loss or fluctuations
Obsession with food, weight, or body shape
Restrictive eating habits or extreme dieting
Frequent episodes of binge eating
Compulsive exercising
Excessive preoccupation with body image
Social withdrawal or isolation
Mood swings or irritability
Body dissatisfaction
Distorted perception of body size
If you or someone you know is experiencing these warning signs, it's important to reach out for help and support.
The Role of Mental Health Professionals
Seeking professional help is essential for the diagnosis, treatment, and management of eating disorders. Mental health professionals, such as psychiatrists, psychologists, and therapists, play a crucial role in the recovery process. They provide:
- Diagnostic assessments to determine the specific type and severity of the eating disorder.
- Individualized treatment plans that may incorporate therapy, counseling, and medication.
- Support and guidance to address underlying psychological, emotional, and behavioral factors contributing to the eating disorder.
- Education and tools to develop healthy coping mechanisms and improve self-esteem.
- Continuous monitoring and follow-up to ensure progress and make necessary adjustments to the treatment plan.
It's important to find a mental health professional who specializes in eating disorders and has experience working with individuals facing these challenges.
Resources for Recovery
Recovery from an eating disorder requires a comprehensive approach that may involve a combination of professional help, support from loved ones, and access to helpful resources. Here are some resources that can aid in the recovery process:
Resources
Support groups: Joining support groups, either in-person or online, provides a safe space to connect with others who understand the challenges of eating disorders.
Helplines: Helplines and crisis hotlines offer immediate assistance and support for individuals in distress.
Treatment centers: Inpatient or outpatient treatment centers specializing in eating disorders can provide intensive support and structured treatment plans.
Educational materials: Books, websites, and online resources can provide valuable information and guidance on understanding and managing eating disorders.
Nutritionists and dietitians: Working with professionals who specialize in eating disorders can help develop healthy eating habits and create an individualized meal plan.
Remember, recovery is a journey that takes time and patience. With the right support network, access to resources, and professional help, individuals struggling with eating disorders can find their path to healing and reclaim a healthy relationship with food and their bodies.
Conclusion
Eating disorders are complex and serious mental health conditions that can have devastating effects on an individual's physical, emotional, and social well-being. While anorexia nervosa, bulimia nervosa, binge eating disorder, and other specified feeding or eating disorders (OSFED) each have unique diagnostic criteria and symptoms, they all share common underlying factors such as genetic predisposition, psychological issues, cultural influences, and environmental stressors.
It's important to recognize the warning signs of an eating disorder and seek professional help from mental health professionals who specialize in treating these conditions. With appropriate treatment and support, individuals with eating disorders can work towards recovery and improve their overall quality of life. Remember that recovery is a journey that takes time and patience, but it is possible with the right resources and support network. By increasing awareness about eating disorders and promoting access to effective treatments, we can help individuals overcome these challenges and achieve lasting wellness.
