Outline of Treatments for Drug Abuse

Overview of Addiction Treatment
Addiction is a complex condition that requires comprehensive and individualized treatment approaches. Treatment for drug abuse typically involves a combination of behavioral therapies and medications. These approaches aim to address the physical, psychological, and social aspects of addiction, helping individuals recover and maintain long-term sobriety.
The Importance of Treatment
Seeking treatment for drug abuse is crucial for several reasons. Firstly, addiction is a chronic condition that can have severe consequences on an individual's physical and mental health, relationships, and overall quality of life. Treatment provides an opportunity for individuals to break free from the cycle of addiction and regain control over their lives.
Secondly, untreated addiction can lead to further complications, including co-occurring mental health disorders, financial difficulties, legal issues, and strained relationships. Effective treatment can help individuals manage these challenges and improve their overall well-being.
Lastly, treatment offers a supportive and structured environment where individuals can learn and develop the necessary skills to overcome addiction. It provides a safe space for individuals to explore the underlying causes of their addiction and develop healthy coping mechanisms, leading to lasting recovery.
Components of Addiction Treatment
Addiction treatment consists of various components that work together to address the complex nature of addiction. These components may vary depending on the individual's specific needs and the treatment program.
- Behavioral Therapies: Behavioral therapies play a crucial role in addiction treatment. These therapies help patients modify their attitudes and behaviors related to drug use, enhance healthy life skills, and persist with other forms of treatment. Some commonly used behavioral therapies include:
- Cognitive-Behavioral Therapy (CBT)
- Contingency Management
- Motivational Enhancement Therapy (MET)
- Family Therapy
- Medications: Medications are often used as part of addiction treatment to help manage withdrawal symptoms, reduce cravings, and prevent relapse. Medications are available for various substance addictions, including opioids and alcohol. The selection of medications and dosages depends on individual needs, and careful consideration is given to potential side effects and interactions.
- Treatment Programs and Settings: Treatment programs and settings provide different levels of care based on the individual's needs. Some common treatment programs and settings include:
- Detoxification (Detox): This initial phase helps patients safely withdraw from substances under medical supervision.
- Residential Treatment: In residential treatment programs, individuals live onsite and receive intensive therapy and support.
- Outpatient Programs: Outpatient programs offer flexibility, allowing individuals to receive treatment while continuing with their daily lives.
- Aftercare Planning: Aftercare planning ensures continuity of care and support after completing a treatment program, helping individuals maintain their recovery [1].
- Integrated Treatment for Co-occurring Disorders: It is common for individuals with substance abuse disorders to have co-occurring mental health conditions. Integrated treatment approaches address both substance abuse and mental health disorders concurrently, providing comprehensive care. This approach recognizes the interconnectedness of these conditions and aims to provide holistic care to improve overall well-being.
By incorporating these components into addiction treatment, individuals are provided with a comprehensive and personalized approach to address their unique needs. It is important to remember that addiction treatment is a journey, and ongoing support and follow-up care are crucial for maintaining long-term recovery.
Medications for Addiction Treatment
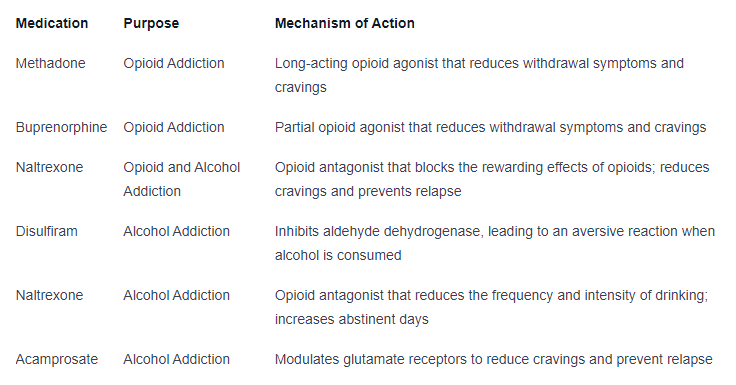
In the comprehensive approach to treating drug abuse, medications play a vital role alongside behavioral therapies. Medications can help manage withdrawal symptoms, reduce cravings, and prevent relapse. Let's explore the medications commonly used for opioid addiction and alcohol addiction, as well as important considerations in medication selection.
Medications for Opioid Addiction
For individuals struggling with opioid addiction, several medications have proven effective in supporting recovery. These medications work by reducing withdrawal symptoms and cravings without inducing euphoria. The three main medications used for opioid addiction are:
- Methadone: Methadone has been successfully used for over 40 years to treat opioid use disorder. It must be administered through specialized treatment programs due to its potential for misuse. Methadone helps individuals maintain abstinence from heroin or prescription opioids by reducing withdrawal symptoms and cravings. It acts as a long-acting opioid agonist, satisfying the brain's need for opioids without producing the intense high associated with other opioids [2].
- Buprenorphine: Buprenorphine is a partial opioid agonist that is as effective as methadone in treating opioid use disorders. It was approved by the FDA in 2002, expanding access to treatment as eligible certified physicians can prescribe it. Buprenorphine also reduces withdrawal symptoms and cravings, allowing individuals to stabilize their lives and engage in counseling and other supportive therapies.
- Naltrexone: Naltrexone is an opioid antagonist that blocks the activation of opioid receptors, thereby preventing rewarding effects like euphoria. It is available in an injectable, long-acting form (Vivitrol®) that was approved in 2010. Naltrexone helps to treat opioid use disorder by reducing cravings and preventing relapse. Compliance with naltrexone medication is crucial for its effectiveness, as regular intake is required to provide continuous protection against relapse [2].
Medications for Alcohol Addiction
Medications are also available to aid individuals in their recovery from alcohol addiction. These medications can help reduce cravings and prevent relapse. The following medications are commonly used:
- Disulfiram (Antabuse): Disulfiram inhibits aldehyde dehydrogenase, resulting in an aversive reaction (sweating, nausea, etc.) when alcohol is consumed. It is used as an adjunctive pharmacotherapy in an abstinence-oriented treatment setting to deter alcohol use and relapse. The aversive reaction serves as a deterrent, discouraging individuals from drinking alcohol by associating it with unpleasant effects.
- Naltrexone: Naltrexone is an opioid antagonist that can be used for the long-term treatment of alcohol dependence. It reduces the frequency and intensity of drinking, lowers the risk of relapse to heavy drinking, and increases the percentage of days abstinent. Compliance with naltrexone medication is a significant factor in its effectiveness as regular intake is necessary to maintain its anti-craving effects.
- Acamprosate (Campral): Acamprosate is an FDA-approved relapse-prevention medication for alcohol dependence. It modulates glutamate receptors, decreasing cravings to drink that may arise from the desire to alleviate withdrawal symptoms. The efficacy of acamprosate has shown mixed results, with more positive outcomes in European studies compared to U.S. studies. It may be more beneficial for patients with severe dependence and higher motivation [3].
Medication Selection and Considerations
The selection of medications for addiction treatment should be based on individual needs and circumstances. Factors to consider include the type and severity of addiction, medical history, potential interactions with other medications, and patient preferences. It is essential to consult with a healthcare professional or addiction specialist to determine the most appropriate medication for each individual.
Table: Medications for Addiction Treatment
When used in conjunction with behavioral therapies, medications can significantly enhance the effectiveness of addiction treatment. It is important to remember that medication-assisted treatment should be provided as part of a comprehensive approach that addresses the physical, psychological, and social aspects of addiction.
Behavioral Therapies for Addiction Treatment
When it comes to treating drug abuse and addiction, behavioral therapies play a crucial role in helping individuals recover and maintain sobriety. Several evidence-based behavioral therapies have shown effectiveness in addressing drug addiction and its underlying factors. In this section, we will explore four commonly used behavioral therapies: Cognitive-Behavioral Therapy (CBT), Contingency Management, Motivational Enhancement Therapy (MET), and Family Therapy.
Cognitive-Behavioral Therapy (CBT)
Cognitive-Behavioral Therapy (CBT) is a widely recognized and extensively studied therapy for drug abuse and dependence. It focuses on identifying and changing negative thought patterns and behaviors related to substance abuse. By addressing the connections between thoughts, feelings, and behaviors, CBT helps individuals develop coping mechanisms and problem-solving skills to overcome drug addiction.
CBT is a structured therapy that typically involves individual or group sessions. It aims to promote self-awareness, identify triggers and high-risk situations, and develop effective strategies to manage cravings and prevent relapse. Through CBT, individuals can gain the necessary skills to resist drugs, cope with stress, and make healthier choices for long-term recovery.
Contingency Management
Contingency Management is a behavioral therapy that utilizes positive reinforcement to encourage drug abstinence and promote desired behaviors. This approach involves providing incentives or rewards for meeting specific behavioral goals, such as drug-free urine tests or attendance at therapy sessions. The rewards can range from vouchers for goods and services to privileges within a treatment program [4].
Research has shown that positive incentives are more effective than negative consequences in producing improved substance use outcomes and retention in treatment. Contingency Management helps to reinforce abstinence and motivate individuals to continue their journey towards recovery. By providing tangible rewards, it encourages individuals to make positive changes and reinforces the belief that recovery is achievable.
Motivational Enhancement Therapy (MET)
Motivational Enhancement Therapy (MET) is a goal-oriented and empathetic therapy that aims to enhance motivation for change in substance use disorders. MET is typically offered in individual or group formats and employs techniques such as active listening, reflective statements, and open-ended questions to explore and resolve ambivalence towards drug use.
The goals of MET include increasing self-motivation, building confidence in the ability to change, and resolving any conflicts or concerns individuals may have regarding their drug use. Through MET, individuals can gain a deeper understanding of the impact of their substance use, explore their values and aspirations, and develop a strong commitment to change.
Family Therapy
Drug addiction not only affects the individual but also has a significant impact on their family and interpersonal relationships. Family Therapy recognizes the importance of involving the family unit in the treatment process. It aims to improve communication, address dysfunctional patterns, and provide support for both the individual with substance abuse issues and their family members.
Family Therapy helps to strengthen family bonds, enhance problem-solving skills, and improve family dynamics. By involving loved ones in the treatment process, individuals with drug addiction can receive the necessary support and encouragement needed for their recovery journey. Family Therapy can also address underlying family issues that may contribute to or result from substance abuse.
These behavioral therapies offer valuable tools and techniques to address drug addiction and support individuals in their recovery process. Each therapy has its own unique approach and benefits, but they all share the common goal of helping individuals overcome drug abuse and sustain long-term sobriety. The choice of therapy depends on the individual's needs, preferences, and the recommendations of healthcare professionals.
Treatment Programs and Settings
When it comes to treating drug abuse, various treatment programs and settings are available to address the physical, psychological, emotional, and social aspects of addiction. These programs are designed to provide individuals with the necessary support and tools to overcome their substance use disorders. Let's explore some of the key treatment programs and settings commonly used in addiction treatment.
Detoxification (Detox)
Detoxification, commonly referred to as detox, is often the first step in addiction treatment. It involves safely withdrawing from substances under medical supervision. The primary goal of detox is to help individuals manage the physical and psychological symptoms associated with withdrawal. Detox programs provide a supportive environment where individuals can safely navigate the initial stages of recovery.
During detox, medical professionals may administer medications to alleviate withdrawal symptoms and ensure the individual's safety. The duration of detox varies depending on the substance involved and the individual's unique circumstances. Detox is typically followed by further treatment and support to address the underlying causes of addiction.
Residential Treatment
Residential treatment programs, also known as inpatient programs, offer intensive therapy and support in a structured environment. These programs provide individuals with a safe and supportive space to focus on their recovery, away from the triggers and temptations of their everyday lives. Residential treatment often includes individual counseling, group therapy, educational programs, and other therapeutic activities.
The duration of residential treatment can vary depending on the individual's needs and the severity of their addiction. Some programs may last for a few weeks, while others may extend to several months. The immersive nature of residential treatment allows individuals to receive comprehensive care and develop essential skills for long-term recovery.
Outpatient Programs
Outpatient programs offer flexibility for individuals seeking treatment for drug abuse. These programs typically involve regular therapy sessions, counseling, and support groups, allowing individuals to receive treatment while still maintaining their daily responsibilities and routines. Outpatient programs are suitable for individuals with less severe substance use disorders or those who have completed a higher level of care, such as residential treatment.
Outpatient treatment may include various components, such as individual therapy, group counseling, and family therapy. These programs provide ongoing support, education, and relapse prevention strategies. The frequency and duration of outpatient sessions depend on the individual's needs and progress in recovery.
Aftercare Planning
Aftercare planning is an essential component of addiction treatment, ensuring continuity of care and support after completing a treatment program. It involves developing a personalized plan that may include ongoing therapy, support groups, medication management, and other resources to help individuals maintain their recovery and prevent relapse.
Aftercare plans are tailored to the individual's specific needs and circumstances. These plans may involve regular check-ins with a therapist, participation in support groups such as 12-step programs or other recovery support networks, and the implementation of healthy coping strategies. The goal of aftercare planning is to provide individuals with the necessary support and resources as they transition back into their daily lives.
By utilizing a combination of detoxification, residential treatment, outpatient programs, and aftercare planning, individuals can receive comprehensive care throughout their recovery journey. These treatment programs and settings aim to address the physical, emotional, and social aspects of addiction, empowering individuals to achieve long-term sobriety and a healthier, more fulfilling life.
Integrated Treatment for Co-occurring Disorders
When it comes to addressing drug abuse and mental health disorders, an integrated treatment approach is crucial. Integrated treatment aims to provide comprehensive care by addressing both substance abuse and mental health simultaneously. This approach recognizes the interconnectedness of these conditions and the need for a holistic treatment plan.
Addressing Mental Health and Substance Abuse
Individuals with co-occurring disorders, which involve both substance abuse and mental health conditions, require specialized treatment that addresses both aspects of their health. Integrated treatment approaches offer a comprehensive approach to address the complex needs of these individuals. By treating both mental health and substance abuse disorders concurrently, individuals can achieve better overall outcomes and improved quality of life.
Integrated treatment typically involves a multidisciplinary team of healthcare professionals, including psychiatrists, psychologists, addiction specialists, and other mental health professionals. This team collaborates to develop an individualized treatment plan that addresses the unique needs and challenges of each person.
One of the key benefits of integrated treatment is the coordination of care between mental health and substance abuse professionals. This ensures that treatment approaches are aligned and that there is a seamless integration of services. By addressing both disorders simultaneously, individuals can experience enhanced recovery outcomes and reduced risk of relapse.
Comprehensive Care Approach
A comprehensive care approach is at the core of integrated treatment for co-occurring disorders. This approach recognizes that individuals with co-occurring conditions require a range of services to support their recovery journey. The comprehensive care model may include a combination of medication-assisted treatment, behavioral therapies, support groups, and other evidence-based interventions.
The National Institute on Drug Abuse (NIDA) has played a significant role in advancing the development and dissemination of behavioral therapies for drug abuse and co-occurring disorders. The introduction of a stage model by NIDA has helped improve the range and rigor of clinical behavioral sciences in this field. This model includes pilot testing of new therapies, evaluation of fully developed treatments, and addressing implementation issues in community settings.
By adopting an integrated treatment approach and utilizing a comprehensive care model, individuals with co-occurring disorders can access the support and interventions necessary for their recovery. This approach recognizes the unique challenges faced by individuals with co-occurring conditions and provides them with a comprehensive and tailored treatment plan to address their specific needs. Integrated treatment offers hope and the opportunity for individuals to achieve lasting recovery and improved overall well-being.
Cognitive-Behavioral Therapy (CBT) for Drug Abuse
Cognitive-Behavioral Therapy (CBT) has emerged as a highly effective treatment approach for individuals struggling with substance use disorders. It encompasses a range of techniques and strategies to address the complex nature of drug abuse and dependence. In this section, we will explore the fundamentals of CBT, its effectiveness, and its applications in drug abuse treatment.
Understanding CBT
CBT is a therapeutic approach that combines cognitive and behavioral techniques to help individuals identify and modify their thoughts, beliefs, and behaviors related to substance abuse. It aims to address the reinforcing effects of psychoactive substances through operant learning strategies, cognitive restructuring, motivation enhancement, and skills-building interventions.
By working collaboratively with a trained therapist, individuals learn to recognize and challenge negative thought patterns, develop healthier coping mechanisms, and acquire skills to resist substance cravings. CBT also helps individuals identify triggers and develop strategies to manage high-risk situations.
Effectiveness of CBT
Numerous studies have demonstrated the efficacy of CBT as both a stand-alone treatment and as part of a comprehensive approach to substance use disorders [4]. CBT has been found to be effective in reducing substance abuse, promoting abstinence, improving treatment retention, and enhancing overall psychological well-being.
Research has shown that CBT can be tailored to address various substances of abuse, including opioids, alcohol, cocaine, and marijuana. It has also been effective in treating co-occurring mental health disorders, such as depression and anxiety, which often accompany substance use disorders.
Applications of CBT
CBT can be applied in different treatment settings, including individual therapy, group therapy, and intensive outpatient programs. It can be used as a primary treatment modality or in combination with other approaches, such as medication-assisted treatment.
In CBT sessions, individuals work with their therapist to set specific goals and develop personalized treatment plans. They learn to identify and challenge maladaptive thoughts and beliefs that contribute to drug abuse, acquire coping skills to manage cravings and high-risk situations, and develop strategies to prevent relapse.
CBT may also involve homework assignments, such as practicing new coping skills or completing thought records, to reinforce what is learned in therapy sessions. The duration of CBT treatment can vary depending on individual needs and treatment goals.
By equipping individuals with practical tools and strategies, CBT empowers them to take control of their thoughts, behaviors, and ultimately, their recovery journey. It provides a structured and evidence-based approach to overcoming drug abuse and building a foundation for long-term sobriety.
Treatment Settings and Services
When it comes to treating drug abuse, there are various treatment settings and services available to individuals seeking help. These options cater to different needs and levels of care. In this section, we will explore three important components: inpatient and outpatient treatment, medications for opioid use disorders, and recovery support services.
Inpatient and Outpatient Treatment
Inpatient and outpatient treatment are two primary settings for individuals seeking treatment for drug abuse. Each setting offers distinct advantages and is chosen based on the severity of the addiction, individual needs, and treatment goals.
Inpatient Treatment: Inpatient treatment, also known as residential treatment, provides a structured and supportive environment for individuals with more severe substance abuse issues. During inpatient treatment, individuals reside at the treatment facility for a specified period, typically ranging from a few weeks to several months. This setting allows for intensive therapy, counseling, and round-the-clock support from a multidisciplinary team of healthcare professionals. Inpatient treatment is particularly beneficial for individuals who require a high level of care and a break from their everyday environment to focus solely on recovery.
Outpatient Treatment: Outpatient treatment provides more flexibility for individuals who do not require 24-hour supervision or have significant social and familial responsibilities. In outpatient treatment, individuals attend therapy sessions and counseling on a scheduled basis while continuing to live at home and carry out their daily activities. This setting allows individuals to receive treatment while maintaining their work, school, or family commitments. Outpatient treatment may involve individual counseling, group therapy, educational services, and other support services. It provides ongoing support and helps individuals transition back into their daily lives while maintaining their recovery progress.
Medications for Opioid Use Disorders
Medications can play a crucial role in the treatment of opioid use disorders. Medications for Opioid Use Disorders (MOUD) are used in conjunction with counseling and other treatment services to support individuals in their recovery journey.
Types of MOUD: There are several types of medications used for opioid addiction treatment. These medications work in different ways to reduce cravings, alleviate withdrawal symptoms, and prevent relapse. Common medications for opioid use disorders include:
- Methadone: A long-acting opioid agonist that helps manage cravings and withdrawal symptoms. It is usually dispensed in specialized clinics.
- Buprenorphine: A partial opioid agonist that can be prescribed by qualified healthcare providers in office-based settings. It helps reduce cravings and withdrawal symptoms.
- Naltrexone: An opioid antagonist that blocks the effects of opioids and reduces cravings. It can be administered in pill form or as a monthly injection.
Considerations for MOUD: The selection of the appropriate medication for an individual with an opioid use disorder depends on various factors, including the severity of the addiction, individual needs, and medical history. It is essential to work closely with a healthcare provider to determine the most suitable medication and dosage for each individual.
Recovery Support Services
Recovery support services play a vital role in the long-term success of individuals in recovery from drug abuse. These services provide ongoing support, guidance, and resources to help individuals maintain their recovery and improve their overall well-being.
Types of Recovery Support Services: Recovery support services encompass a wide range of services aimed at improving individuals' quality of life and assisting them in their recovery journey. These services may include:
- Individual counseling: One-on-one counseling sessions to address specific challenges, develop coping strategies, and enhance overall well-being.
- Group counseling: Participating in therapy sessions with peers facing similar challenges, providing support, and fostering a sense of community.
- Educational services: Workshops, classes, and educational resources to enhance understanding of addiction, relapse prevention, and healthy lifestyle choices.
- Vocational services: Assistance with job search, career development, and skills training to promote financial stability and independence.
- Life skills training: Programs that teach essential life skills such as budgeting, time management, and stress management to support individuals in their recovery and daily lives.
- Mental health treatment for co-occurring disorders: Addressing underlying mental health issues alongside substance abuse to ensure comprehensive care.
- Family services: Involving family members in the recovery process through counseling, education, and support groups to rebuild healthy relationships and promote a supportive environment.
- Continuing care: Planning for ongoing support and services after completing initial treatment, including recovery houses, sober dorms, recovery high schools, and recovery support groups, to maintain long-term recovery and prevent relapse.
By combining different treatment settings and services, individuals can access comprehensive care tailored to their specific needs. Whether through inpatient or outpatient treatment, utilizing medications for opioid use disorders, or engaging in various recovery support services, individuals can find the appropriate level of care and support on their path to recovery.
Group Therapy for Substance Use Disorders
Group therapy is a valuable treatment modality for individuals with substance use disorders. It provides an opportunity for individuals to interact with others facing similar challenges and receive support from their peers. In this section, we will explore the matching of group therapy models, the goals of group therapy, and the benefits it offers.
Matching Group Therapy Models
Group therapy models should be matched with the needs of the particular population being treated and the goals of the group's treatment [7]. Different group therapy models exist, such as cognitive-behavioral therapy (CBT), contingency management, motivational enhancement therapy (MET), and family therapy. Each model has its own approach and focus, allowing treatment providers to select the most appropriate model based on the specific needs and characteristics of the participants.
Goals of Group Therapy
The primary goal of group therapy for substance use disorders is to provide a supportive and therapeutic environment where individuals can explore their thoughts, feelings, and behaviors related to substance abuse. Some common goals of group therapy include:
- Encouraging mutual support and empathy among participants
- Enhancing motivation for change and maintaining abstinence
- Developing effective coping strategies and relapse prevention skills
- Promoting healthy communication and interpersonal skills
- Addressing underlying emotional issues and trauma that contribute to substance use
By working together within a group setting, individuals can gain insights, share experiences, and learn from one another's successes and challenges.
Benefits of Group Therapy
Group therapy offers several benefits that can contribute to the recovery process for individuals with substance use disorders. These benefits include:
- Shared Experience and Support: Group therapy provides a sense of belonging and support by connecting individuals who are going through similar struggles. It allows participants to share their experiences, offer insights, and provide support to one another.
- Learning from Peers: Group therapy offers the opportunity to learn from others who have successfully overcome substance abuse. Participants can gain valuable insights, coping strategies, and relapse prevention techniques from their peers.
- Social Skills Development: Group therapy provides a safe space for individuals to practice healthy communication, active listening, and conflict resolution skills. These skills can then be applied to their relationships outside of the therapy setting.
- Increased Accountability: Being part of a group creates a sense of accountability, as participants can share their progress, setbacks, and goals with others. This accountability can serve as a motivator for maintaining sobriety and making positive changes.
- Normalization of Experiences: Group therapy helps individuals realize that they are not alone in their struggles. Hearing others' stories and challenges can normalize their own experiences and reduce feelings of shame and isolation.
- Cost-Effective Treatment: Group therapy is often more cost-effective compared to individual therapy, making it more accessible for individuals seeking treatment for substance use disorders.
Group therapy, when conducted by trained professionals, can be a powerful treatment approach that complements other forms of treatment for substance use disorders. It provides a supportive and non-judgmental environment where individuals can gain valuable insights, learn new skills, and build a network of support to aid their recovery journey.
References
[1]: https://americanaddictioncenters.org/therapy-treatment
[2]: https://nida.nih.gov/publications/research-reports/medications-to-treat-opioid-addiction/how-do-medications-to-treat-opioid-addiction-work
[3]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3767185/
[4]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3633201/
[5]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2897895/
[6]: https://www.va.gov/WHOLEHEALTHLIBRARY/tools/substance-use-disorder-treatment-complementary-approaches.asp
